This post was originally published on this site
Therapeutics that target brain immune cells known as microglia may prevent the formation of amyloid-beta plaques, one of the hallmarks of Alzheimer’s disease, according to a recent mouse study.
The study, ”Sustained microglial depletion with CSF1R inhibitor impairs parenchymal plaque development in an Alzheimer’s disease model,” was published in the journal Nature Communications.
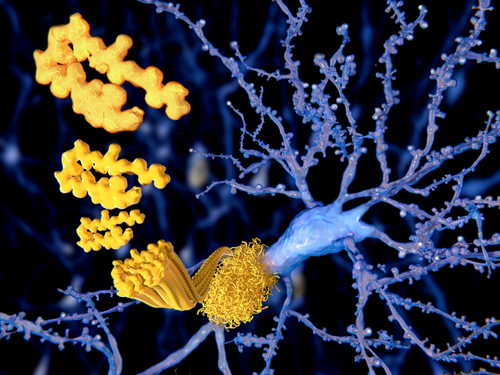
Alzheimer’s disease is characterized by the formation of amyloid-beta protein aggregates (plaques) that accumulate between nerve cells in the brain, disrupting their function.
Microglia, the immune cells of the central nervous system (brain and spinal cord), are responsible for maintaining cell balance within the brain. They release pro- and anti-inflammatory signals in response to changes in the brain’s microenvironment, clearing amyloid-beta aggregates in the brain and contributing to the health of the brain’s neuronal network.
Microglia have been implicated in Alzheimer’s disease. Research has shown that removal of microglia from mouse models of Alzheimer’s during the advanced stages of the disease — when there is an extensive build-up of amyloid-beta plaques — protected against the loss of neurons and synapses (the junctions between two nerve cells that allow them to communicate).
Furthermore, most of the genes associated with an increased risk of developing Alzheimer’s are active in microglia. Despite this evidence, the exact role of microglia in the earlier stages of the disease is not well-understood.
“[W]e hadn’t understood exactly what the microglia are doing and whether they are significant in the initial Alzheimer’s process,” Kim Green, associate professor of neurobiology and behavior at the University of California, Irvine School of Biological Sciences and the study’s lead author, said in a press release.
“We decided to examine this issue by looking at what would happen in their absence.”
Researchers developed an oral inhibitor, called PLX5622, that specifically targets the colony-stimulating factor 1 receptor (CSF1R), an essential protein for the survival of microglia. This inhibitor was able to penetrate the brain and reach the microglia.
The inhibitor was given to a mouse model of Alzheimer’s disease that begins to form amyloid-beta plaques by three months of age. The first oral administration was given at 1.5 months of age and treatment was kept from 10 up to 24 weeks.
Compared to wild-type (control) mice, PLX5622 eliminated microglia almost completely in the Alzheimer’s mouse model (an elimination between 97 to 100%). Importantly, removal of microglia impaired the formation of amyloid-beta plaques.
“What was striking about these studies is we found that in areas without microglia, plaques didn’t form,” Green said. “In places where microglia survived, plaques did develop.”
The plaques that still developed in specific brain regions were associated with a subset of microglia that initially were resistant to PLX5622.
Overall, these findings suggest that formation of amyloid-beta plaques requires the presence and activity of microglia.
“You don’t have Alzheimer’s without plaques, and we now know microglia are a necessary component in the development of Alzheimer’s,” Green said.
Further analysis showed that gene activity in the hippocampus, a brain region linked to memory and spatial navigation, was altered in Alzheimer’s mice. Specifically, researchers found a lower activity of genes important for neuronal function and synapses.
Removal of microglia rescued the changes in gene expression, even though plaques were still present in the hippocampus. These findings suggest that while attacking amyloid-beta plaques, microglia switch off genes that are important for neuronal function. (Of note, gene expression is the process by which information in a gene is synthesized to create a working product, such as a protein.)
“This finding underlines the crucial role of these brain immune cells in the development and progression of Alzheimer’s,” Green said.
This discovery indicates that microglia may be an important therapeutic target in Alzheimer’s disease. However, given the importance of them in regulating other brain functions, future therapies must target microglia in a specific manner rather than causing their widespread removal.
“We are not proposing to remove all microglia from the brain,” Green said. “What could be possible is devising therapeutics that affect microglia in targeted ways.”
The team believes these results show that microglia contribute to several aspects of Alzheimer’s: they are crucial during the initial phase, where plaques begin to form, after which they promote a chronic inflammatory state that modulates alterations in neuronal gene expression in response to amyloid-beta accumulation.
Moreover, because microglia play a role in other brain diseases, their potential targeted elimination also could become a therapeutic strategy in disorders other than Alzheimer’s.
“These immune cells are involved in every neurological disease and even in brain injury,” Green added. “Removing microglia could enable researchers working in those areas to determine the cells’ role and whether targeting microglia could be a potential treatment.”
The post Carefully Targeting Brain Immune Cells May Help Prevent Amyloid-beta Plaques, Study Suggests appeared first on Alzheimer’s News Today.
The post Carefully Targeting Brain Immune Cells May Help Prevent Amyloid-beta Plaques, Study Suggests appeared first on BioNewsFeeds.